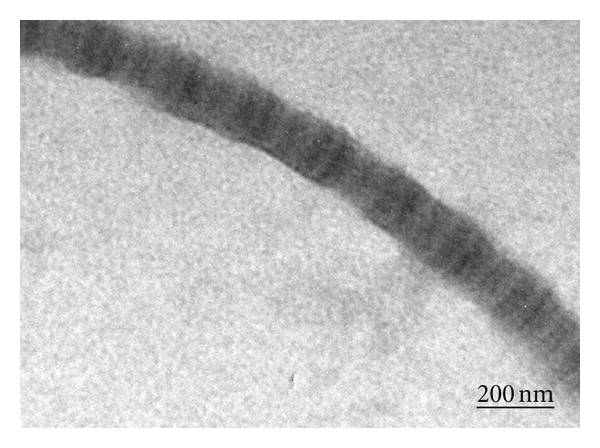
Electrospun scaffold has been established as a biocompatible form for regenerative scaffold. Its high porosity and fibrous nature allows nutrient transfer and structural integrity. Wide range of material selection and versatility of the process has given researchers a range of options to choose from in the development of implantables. These options may not be mutually exclusive and each has its own advantages and disadvantages.
Biodegradable and non-biodegradable
In recent decades, there is much interest in biodegradable polymers. Biodegradable polymers are attractive for use as implantable scaffolds as the eventual replacement of the scaffold by host tissues will eliminate or reduce any long term foreign body response complications, however, there a few complications when using biodegradable polymers. The most tricky is the maintenance of adequate mechanical properties as it degrades in vivo. Unexpected accelerated degradation of the polymer may cause the implant to fail prematurely. It is also important to note the by products of the degraded polymer and its effect on its immediate environment. Lactic acid-based polymers are known to increase the acidity of its surrounding as it degrades into acid. This is made worse if the acidic by-products accumulate within the scaffold causing accelerated degradation and subsequent inflammatory reactions. In this case, electrospun fibers may have an advantage. Degradation rate of PLGA has been shown to be slower in its electrospun form compared to film [Shang et al 2010]. This may seem counter-intuitive as higher surface area of nanofibers should result in faster degradation rate. Presence of catalytic by-products trapped within a block material may increase its degradation rate compared to highly porous nanofibers where by-products are quickly released into the media as in the case of PLGA. Natu et al (2012) did a long term (30 months) comparison of the degradation rate of PCL material produced by different methods, electrospinning, solvent casting, melt compression and supercritical fluid processing. Their result showed that in the first year, degradation rate was consistently slowest for electrospun fibers compared to the materials produced by the other three methods. However, at 30 months, the molecular weight of the electrospun nanofibers was almost the same as the materials produced using other methods.
Non-biodegradable products in contrast are more stable in terms of maintaining its properties. There are also a wider range of materials to choose from with their own unique characteristics. Due to the absence of degraded products, biocompatability can be assured and its performance more predictable. Its main limitation is the continued presence of the foreign material may cause a gradual rejection of the implant by the body in the long run.
The selection of either biodegradable or non-biodegradable material in specific medical applications is subjected to risk analysis. Where premature mechanical failure would be catastrophic, non-biodegradable material or very slow biodegradable material would reduce the risk. The age of the patient may also play a part in material selection. For younger patients, biodegradable materials may be better as the body may reject non-biodegradable material in the long run which may necessitate a corrective surgery.
Cellular and Acellular
Implantable scaffolds are currently dominated by acellular grafts due to the challenge and the cost of having cells in the scaffold prior to implantation. Numerous studies have shown that having cells seeded into the scaffold prior to implantation yields better results than acellular graft. This can be attributed to additional cells in the scaffold kickstarting the healing process instead of waiting for the appropriate host cells to populate the scaffold. Conventional method of having scaffold seeded with cell involves harvesting the cells, expansion of the cell population in vitro and seeding into the scaffold followed by implantation. Research is underway to reduce the time taken to expand the cell population by using stem cells. Stem cells can be isolated from bone marrow or adipose tissue and quickly seeded in the scaffold for implantation or grafting within a single surgical session. This is where electrospun scaffold has demonstrated its usefulness. Research has shown that electrospun membrane is able to quickly capture stem cells. Studies have shown that 25% of hematopoietic stem cell (HSC) was captured on collagen and PLGA/collagen blend in 30 min as compared to only about 2% on TCP[Ma et al 2008]. Significantly higher percentage of MSC was also found to adhere on electrospun membrane at 1 hour (50 to 71%) compared to smooth film (28%) of the same material [Finne-Wistrand et al 2008].
Synthetic and Natural materials
Many naturally occurring polymers and proteins have been shown to be better substrate for cell viability compared to synthetic materials. Its main limitation is the batch to batch consistency in the material properties. Proteins such as collagen are part of natural extracellular matrix and have consistently showed good cell adhesion and proliferation results in vitro. However, its rapid degradation is a major limitation if it is to last more than a few weeks when implanted. Special care may also be needed in the use of some natural polymers due to concerns with disease transfers. Mechanical properties of most natural polymers are also often weaker than synthetic polymers.
A significant advantage of synthetic polymers is that they can be easily tailored to meet implant requirements. Rate of biodegradation and other properties can be controlled through raw material selection and its processing. There is also greater consistency in its characteristics unlike natural polymers which may vary greatly between batches.
To take advantage of better cell response to natural polymers and greater consistency and mechanical properties of synthetic polymers, materials have been used together. Collagen type I has been shown to be electrospinnable [Matthews 2002] however, it is not always possible due to difference in raw material source and its processing conditions. When collagen is mixed with electrospinnable synthetic polymers, it is almost always possible to get fibers. Cell response to such mixed material electrospun fibers may be comparable to scaffold from pure collagen. Mixing of natural polymers with synthetic polymers also allows low molecular weight polymers such as GAG to be incorporated into fibers. Studies have shown that synthetic fibers blended with collagen showed significantly better cell proliferation compared to pure synthetic fibers [Venugopal et al 2005]. In an in vivo study by Tillman et al (2009) using polycaprolactone/collagen (1:1) blended electrospun vascular graft, the graft was able to maintain a circumferential tensile strength that was comparable to that of native aorta 1 month after implant although the tensile strength was reduced by half from pre-implant samples. The reduction in tensile strength was probably due to the degradation of collagen. PCL is known to exhibit slow biodegradation rate thus it is likely that the mechanical strength of the scaffold is maintained by PCL.
Clinical Application
Electrospun scaffold typically comes in the form of a flat, 2D mesh which is suitable for application such as skin grafts or separation membrane. It may also be formed into tubular structure for applications such as vascular graft or nerve grafts. While it is understood that nanofibrous structure helps in regeneration, there are situations where the tissue or organs are more complex which makes direct application of electrospun scaffold challenging. For the repair of an aortic arch, Mayoral et al (2022) used a hybrid fused deposition modeling (FDM) and electrospinning techniques to construct 2D circular patches which were subsequently reshaped using another 3D printed mold specific to the patient's anatomy. FDM in the hybrid scaffold consisted of a thick grid to provide support and to maintain the final shape. The electrospun nanofiber network fills in the space between the grid and to mimic the extracellular matrices (ECM). Polycaprolactone (PCL) was the material of choice for both FDM and electrospinning as it is known to be biocompatible and it has a low melting point.
Published date: 27 September 2016
Last updated: 13 December 2022
▼ Reference
-
Finne-Wistrand A, Albertsson A C, Kwon O H, Kawazoe N, Chen G, Kang I K, Hasuda H, Gong J, Ito Y. Resorbable Scaffolds from Three Different Techniques: Electrospun Fabrics, Salt-Leaching Porous Films, and Smooth Flat Surfaces. Macromol. Biosci. 2008; 8: 951.
-
Ma K, Chan C K, Liao S, Hwang W Y K, Feng Q, Ramakrishna S. Electrospun nanofiber scaffolds for rapid and rich capture of bone marrow-derived hematopoietic stem cells. Biomaterials 2008; 29: 2096.
-
Matthews J A, Wnek G E, Simpson D G, Bowlin G L. Electrospinning of collagen nanofibers. Biomacromolecules 2002; 3: 232.
-
Mayoral I, Bevilacqua E, Gómez G, Hmadcha A, González-Loscertales I, Reina E, Sotelo J, Domínguez A, Pérez-Alcántara P, Smani Y, González-Puertas P, Mendez A, Uribe S, Smani T, Ordoñez A, Valverde I. Tissue engineered in-vitro vascular patch fabrication using hybrid 3D printing and electrospinning. Materials Today Bio 2022; 14: 100252.
Open Access
-
Natu MV, de Sousa HC, Gil MH, Influence of polymer processing technique on long term degradation of poly(ε-caprolactone) constructs, Polymer Degradation and Stability 2013; 98: 44.
-
Shang S, Yang F, Cheng X, Walboomers X F, Jansen J A. The effect of electrospun fibre alignment on the behaviour of rat periodontal ligaments cells. European Cells and Materials 2010; 19: 180.
Open Access
-
Tillman B W, Yazdani S K, Lee S J, Geary R L, Atala A, Yoo J J. The in vivo stability of electrospun polycaprolactone-collagen scaffolds in vascular reconstruction. Biomaterials 2009; 30: 583.
-
Venugopal J, Ma L L, Yong T, Ramakrishna S. In vitro study of smooth muscle cells on polycaprolactone and collagen nanofibrous matrices. Cell Biology International 2005; 29: 861.
▲ Close list
 ElectrospinTech
ElectrospinTech