▼ Reference
- Baranowska-Korczyc A, Warowicka A A, Jasiurkowska-Delaporte M, Grzeskowiak B, Jarek M, Maciejewska B M, Jurga-Stopa J, Jurga S. Antimicrobial electrospun poly(ε-caprolactone) scaffolds for gingival fibroblast growth. RSC Adv. 2016; 6: 19647.
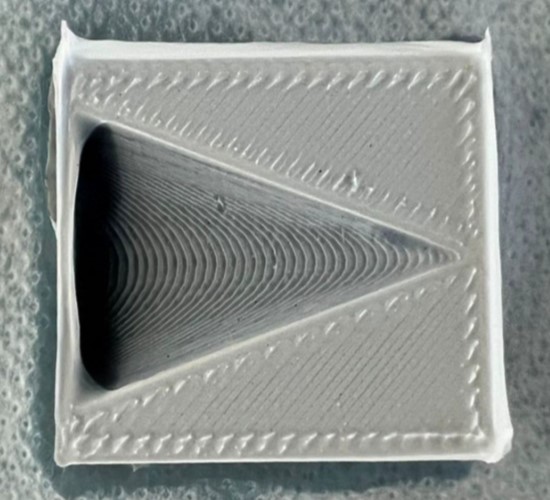
- Bauer L, Brandstäter L, Letmate M, Palachandran M, Wadehn FO, Wolfschmidt C, Grothe T, Güth U, Ehrmann A. Electrospinning for the Modification of 3D Objects for the Potential Use in Tissue Engineering. Technologies. 2022; 10(3):66. https://www.mdpi.com/2227-7080/10/3/66/htm Open Access
- Gholami A, Abdoluosefi H E, Riazimontazer E, Azarpira N, Behnam M, Emami F, Omidifar N. Prevention of Postsurgical Abdominal Adhesion Using Electrospun TPU Nanofibers in Rat Model. BioMed Research International 2021; 2021: 9977142. Open Access
- Han N, Rao S S, Johnson J, Parikh K S, Bradley P A, Lannutti J J, Winter J O. Hydrogel-electrospun fiber mat composite coatings for neural prostheses. Front. Neuroeng. 2011; 4: 2 Open Access
- Iafisco M, Foltran I, Sabbatini S, Tosi G, Roveri N. Electrospun Nanostructured Fibers of Collagen-Biomimetic Apatite on Titanium Alloy. Bioinorganic Chemistry and Applications 2012; 2012: 123953. Open Access
- Li L L , Wang L M, Xu Y, Lv LX. Preparation of gentamicin-loaded electrospun coating on titanium implants and a study of their properties in vitro. Arch Orthop Trauma Surg 2012; 132: 897.
- Liao S, Theodoropoulos C, Blackwood K A, Woodruff M A, Gregory S D. Melt Electrospun Bilayered Scaffolds for Tissue Integration of a Suture-Less Inflow Cannula for Rotary Blood Pumps. Artificial Organs 2017 Article in press
- Luo L, He Y, Chang Q, Xie G, Zhan W, Wang X, Zhou T, Xing M, Lu F. Polycaprolactone nanofibrous mesh reduces foreign body reaction and induces adipose flap expansion in tissue engineering chamber. International Journal of Nanomedicine 2016; 11: 6471. Open Access
- Ravichandran R. Biomimetic Surface Modification of Dental Implant for enhanced Osseointegration. MEng Thesis. National University of Singapore 2009. Open Access
- Shahi R G, Albuquerque M T, Münchow E A, Blanchard S B, Gregory R L, Bottino M C. Novel bioactive tetracycline-containing electrospun polymer fibers as a potential antibacterial dental implant coating. Odontology 2016 Article in press.
- Soujanya G K, Hanas T, Chakrapani V Y, Sunil B R, Kumar T S S. Electrospun Nanofibrous Polymer Coated Magnesium Alloy for Biodegradable Implant Applications. Procedia Materials Science 2014; 5: 817. Open Access
▼ Credit and Acknowledgement
Author
Wee-Eong TEO View profile
Email: weeeong@yahoo.com
 ElectrospinTech
ElectrospinTech