The field of dentistry is very wide including specializations such as endodontics, periodontics and orthodontics. Electrospinning, due to its flexibility in material selection and its ability to produce fibers in the submicron to nanometer dimension, is ideally suited in producing materials for dental applications. Materials used for dental applications are typically found in small volume and size due to the size constrain of the oral cavity. Electrospun materials are been investigated for various dental applications.
Composite
Dental composites are typically filled resins for use as fillers or for bonding purpose. The strong mastication force encountered by the composite requires it to be strong with good fracture properties. Various electrospun fibers have been tested as fillers in dental composites to improve its mechanical properties. As a reinforcement filler, the electrospun fibers need to exhibit good strength and modulus. Karatepe et al (2020) seek to improve the mechanical properties of electrospun poly(methylmethacrylate) (PMMA) fibers for potential incorporation into PMMA based denture resin materials. To add antibacterial functionality into the electrospun fiber, poly(ethyleneimine) (PEI), a hyperbranched cationic polymer was added to the solution to be electrospun. Silk fibroin (SF) was also added to PMMA solution to improve the mechanical strength of electrospun PMMA fibers. Tensile strength of electrospun PMMA/SF mat was weaker than electrospun PMMA only mat while PMMA/PEI mat was found to be stronger. Elastic modulus did not change significantly when either SF or PEI was added to PMMA. Interestingly, the elastic modulus of electrospun PMMA/SF/PEI mat showed a 52% increase in elastic modulus and a two fold increase in tensile strength over PMMA only mat. This has been attributed to the formation of free COOH groups and CN bonds suggesting presence of newly formed bonds. The composite mat was also found to inhibit P. aeruginosa, a rod-shaped gram-negative pathogenic bacterium, which is an oral pathogen. Generally, only a small amount of nanofibers is needed to substantially improve the mechanical properties although beyond an optimal amount, the performance starts to deteriorate. Dodiuk-Kenig et al (2008) used electrospun polyvinyl alcohol, poly-L-lactide and nylon 6 as reinforcement to improve the mechanical property of hyperbranched polymer modified (Hybrane, 0.3 wt.% DSM) dental formulations. Their test showed that the mechanical property is influenced by the fiber diameter, type and concentration. For fiber diameters of 250 nm and 125 nm, there is no apparent trend in its effect on the compressive strength, flexural strength and tensile strength [Dodiuk-Kenig et al 2008]. Tian et al (2007) investigated the reinforcing effect of nylon 6 nanocomposite nanofibers containing highly aligned fibrillary silicate single crystals when blended into 2,2'-bis-[4-(methacryloxypropoxy)-phenyl]-propane (Bis-GMA) / tri- (ethylene glycol) dimethacrylate (TEGDMA) dental composites. With 2% mass fraction of nanofibers impregnated, the composite flexural strength, elastic modulus and work-of-fracture improves by 23%, 25% and 98% respectively. However, when higher mass fraction of nanofibers is impregnated, the mechanical properties dropped. This may be due to inadequate wetting, presence of voids/defects and weakness in the nanofiber filler.
Glass fibers are commonly used as fillers in polymer matrix composite. Electrospinning has been used to produce fibers out of glass precursors and subsequently pyrolyzed to form nano-scaled glass fibers. Gao et al (2008) tested the mechanical properties of Bis-GMA/TEGDMA with 70% fillers comprising of a mixture of electrospun-derived glass fiber and Esstech glass powder. Having a composition of electrospun-derived glass fiber reinforcement at 7.5% such that the total mass fraction of filler remains at 70%, the flexural strength, elastic modulus and work-of-fracture of Bis-GMA/TEGDMA with 70% Esstech glass powder fillers was improved by 44%, 29% and 66% respectively. Other types of electrospun inorganic fibers have also been fabricated with the potential use as fillers in composite. Shah et al (2012) has shown that it is possible to fabricate two dimensional nanofibrous membrane and three dimensional wool-like nanofibrous structures by increasing the ratio of polyethylene oxide (PEO) to silica colloidal solution (30% solid loading) from 80:20 to 50:50 with the former generating two dimensional membrane and the latter, three-dimensional structure. Pyrolysis is used to remove PEO to give pure silica fibers. Proper preparation such as ensuring complete wetting of the nanofiber mesh and removal of air inclusion may be more challenging in a three-dimensional nanofibrous form due to its greater bulk. Poor impregnation of the nanofiber filler in the matrix will result in a composite that is weaker than unfilled resin [Boyd et al 2012].
| Composition |
Fexural Strength |
Elastic modulus |
Work-of-fracture |
Reference |
| Bis-GMA/TEGDMA |
95 MPa |
2 GPa |
4.3 kJ/m2 |
Tian et al 2007 |
| Bis-GMA/TEGDMA with 2.0% (mass fraction) neat nylon 6 nanofiber |
106 MPa |
2.4 GPa |
6.7 kJ/m2 |
Tian et al 2007 |
| Bis-GMA/TEGDMA with 2.0% (mass fraction) neat nylon 6/ fibrillar silicate nanocomposite nanofiber nanofiber |
117 MPa |
2.5 GPa |
8.5 kJ/m2 |
Tian et al 2007 |
| Bis-GMA/TEGDMA with 70% Esstech glass powder |
88 MPa |
4.9 GPa |
6.1 kJ/m2 |
Gao et al 2008 |
| Bis-GMA/TEGDMA with 7.5% silanized electrospun glass fiber and 62.5% Esstech glass powder |
127 MPa |
6.3 GPa |
10.1 kJ/m2 |
Gao et al 2008 |
| Bis-GMA/TEGDMA with 0.3% wt hyperbranch polyesteramide and 0.05 wt% polyvinyl alcohol nanofibers |
357 MPa |
Not tested |
Not tested |
Dodiuk-Kenig et al 2008 |
| Bis-GMA/TEGDMA with 0.3% wt hyperbranch polyesteramide and 0.3 wt% poly-L-lactide nanofibers |
357.3 MPa |
Not tested |
Not tested |
Dodiuk-Kenig et al 2008 |
| Bis-GMA/TEGDMA with 0.3% wt hyperbranch polyesteramide and 0.01 wt% polyamide-6 nanofibers |
257.5 MPa |
Not tested |
Not tested |
Dodiuk-Kenig et al 2008 |
Tissue regeneration
Electrospun nanofiber scaffold with its resemblance to natural extracellular matrix (ECM) is known to facilitate cell adhesion and proliferation. This has prompted research into its use as a scaffold for dental tissue engineering. Of particular interest is the response and biocompatibility of dental pulp stem cells on electrospun scaffold. Dental pulp stem cells have the ability to differentiate and may form dentine-pulp complex which is vital for tooth regeneration. Several studies have shown that dental pulp stem cells is able to adhere and proliferated well on electrospun scaffolds [Deng et al 2007, Yang et al 2010]. Yang et al (2010) showed that electrospun composite scaffolds made of polycaprolactone (PCL)/ gelatin/nano-hydroxyapatite (nHA) and PCL/gelatin was able to support dental pulp stem adhesion, proliferation and odontogenic differenation. In particular the presence of nHA significantly increases odontogenic differenation both in vitro and in vivo.
Eap et al (2014) brought a step closer to tooth regeneration when they successfully reinnervate a bioengineered tooth on electrospun polycaprolactone membrane loaded with neural growth factor. ED14 tooth germs were cultured on electrospun PCL membrane for six days before implanting behind the ears of mice for 2 weeks. Following 2 weeks of implantation, correct development of tooth crown can be seen with secretion of predentin/dentin. Their study showed that without neural growth factor, there is no innervation. In contrast, the presence of growth factor encourages axon growth and innervation of the dental pulp.
Apart from tooth regeneration, other parts of the dental system also play important roles. Tooth supporting structure such as the gingiva, periodontal ligament (PDL), alveolar bone, and root cementum are needed to prevent tooth loss. Yang et al (2019) investigated the use of electrospun polycaprolactone (PCL) as fibre-guiding scaffold for periodontal ligament regeneration. In their study, aligned nanofibers and random nanofibers mesh were tested and gelatin was used for binding several mesh layers together to form a three-dimensional scaffold. Human periodontal ligament mesenchyme cells (PDLSCs) were seeded on both scaffolds and examined for their performance in periodontal ligament regeneration. PDLSCs cultured on aligned PCL 3D nanofiber scaffold showed greater alignment and expresses significantly higher level of periostin when compared with the blank control and random 3D nanofiber scaffold. In vivo study was carried out on a Sprague-Dawley rat periodontal fenestration defect model. At 6 weeks, the aligned 3D scaffold demonstrated much more obvious bone formation at the fenestration defect compared to random 3D scaffold and blank control.
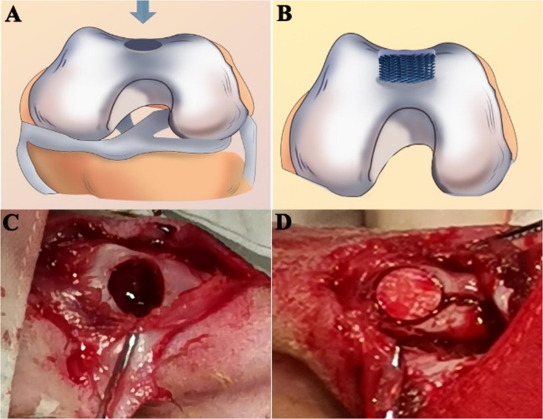
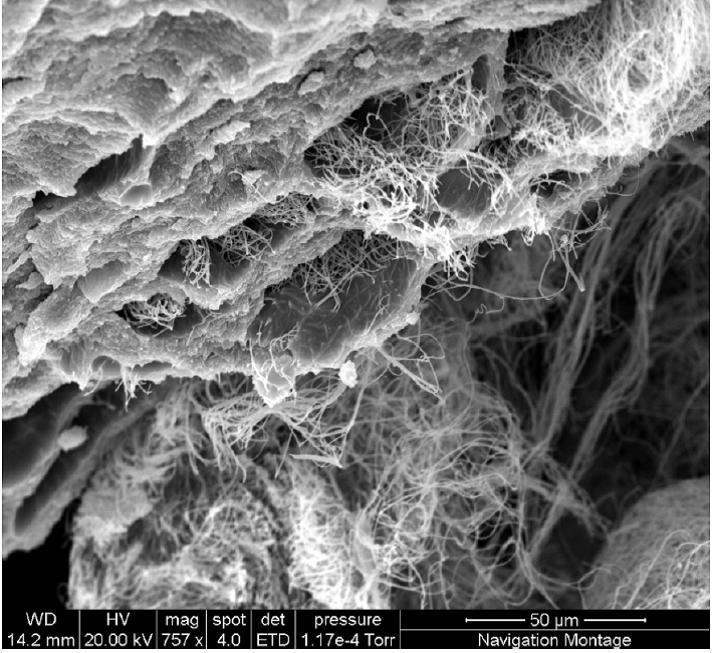
Electrospun fibers have also been used in the construction of scaffolds for periodontal bone regeneration. Liu et al (2021) used electrospinning and 3D printing to construct a hybrid bi-layer scaffold for guided bone regeneration. Polycaprolactone/gelatine (PCL/Gel) nanofibre membranes was first electrospun followed by conjugation with heparin. 3D printing of PCL/Gel/nano-hydroxyapatite (n-HA) scaffold was carried out over the PCL/Gel-heparin membrane to form a bi-layer scaffold. <>In vivo study on a rabbit osteochondral defect model showed that the hybrid bi-layer scaffold group showed a higher degree of new bone formation than the 3D printed PCL/Gel/n-HA scaffold and control group after 5 and 20 weeks. With the electrospun membrane positioned on the surface and the defect filled in by the 3D printed bulk volume, the membrane prevents surrounding fibrous connective tissues from migrating into the bone defect. The inner layer with the 3D printed macropores allows bone regeneration while supporting the surface membrane.
A guided tissue regeneration (GTR) membrane may also be used to replace lost periodontal tissues. This GTR provides a barrier membrane between the gingival epithelium and the underlying periodontal bone to prevent the migration of epithelial cells or gingival fibroblasts to the injury site and disrupts proper healing since progenitor bone and periodontal ligament cells growth rates are slower. Nitti et al (2022) constructed a bilayered poly(lactic-co-glycolic acid) (PLGA)) membrane using dip coating to first form a smooth layer followed by electrospinning to deposit fibers on the layer to give a rough, fibrous layer. The smooth layer functions as a barrier against cell entry while the rough layer may facilitate cell growth. To form aligned fibers, the smooth layer was mounted on a drum and rotated at high speed (2000 rpm) to collect the fibers. For randomly aligned fibers, the drum was rotated at a slower speed (100 rpm). Comparing a single dip coated layer membrane and the bilayered membrane, the bilayered membrane with the electrospun layer showed a much greater water uptake capacity. This can be attributed to the greater porosity of the electrospun layer. In terms of mechanical properties, the bilayered membrane showed significantly greater tensile strength and modulus compared to electrospun only membrane. This can be attributed to the presence of the smooth coated layer.
Enamel Regeneration
Electrospinning can be used to form fiber carrier for various organic and inorganic materials. Fletcher et al (2011) used this advantage of electrospinning to create a mat of amorphous calcium phosphate (ACP)/poly(vinylpyrrolidone)(PVP) nanofibers for remineralization of enamel. In the presence of fluoride, it was shown that ACP phase at the surface of the enamel formed a contiguous overlayer of crystalline fluoridated hydroxyapatite. This is potentially useful for regeneration of enamel and for the alleviation of dentine hypersensitivity amongst others.
Dental implant surface modification
Dental implant is often used as a more permanent fix to replace lost tooth. However, the clinical success of the dental implant is dependent on its osseointegration which is the ability of host tissues to form new bone around the implant. Failure of the implant is often attributed to the formation of fibrous tissues around the implant instead of direct bone contact to the implant surface. As the fibrous tissue is mechanically weak, it is unable to provide long term support for the implant after the healing process is completed. To ensure direct bone contact to the implant surface, one method is to encourage mineral deposition on the implant surface by osteoblast or mesenchymal stem cells. Ravichandran (2009) showed that adhesion of mesenchymal stem cells (MSC) on titanium plate and alloy is significantly enhanced with nanofiber coating even with man-made polymer such as poly(lactic acid)-co-poly(glycolic acid) (PLGA). Incorporation of the PLGA nanofiber with collagen and hydroxyapatite (HA) further increases the adhesion of MSCs on the implant surface. Titanium alloy coated with PLGA/collagen and HA nanofibers showed better proliferation and exhibited significantly greater alkaline phosphatase activity and mineral secretion than untreated titanium alloy.
Dental Pulp Capping
Pulp capping is a technique used to protect dental pulp after it has being exposed during cavity preparation. A favourable outcome is quick formation of dentin bridge over the cavity so that further restorative work can be carried out. Mineral trioxide aggregate (MTA) is commonly used for direct pulp capping. Lee et al (2015) tested the clinical performance of MTA alone and electrospun poly(ε-caprolactone) (PCL) fiber mesh as a barrier for MTA. After 3 months, teeth treated with PCL and MTA formed approximately 3-fold thicker dentin bridge than MTA direct pulp capping. Dentin bridge formation with PCL and MTA was also significantly faster.
Antibiotic film
Ease of incorporating drugs and other additives into electrospun fibers have led to the development electrospun anti-microbial nanofibers for various applications. Large surface area of nanofibers increases the chance of contact and exposure by microbes to the anti-microbial additives. Albuquerque et al (2015) tested the potential use of electrospun scaffold embedded with Ciprofloxacin to reduce infection of the root canal system before regenerative procedures. The efficacy of the drug loaded polydioxanone nanofibers was tested on dentin specimens infected with E. faecalis biofilm. Polydioxanone nanofibers with 25 wt% drug loaded showed no microbial growth after two days while nanofibers without drug showed very high bacterial count.
The progression of periodontitis was known to be caused by microorganisms, Aggregatibacter actinomycetemcomitans, Actinomyces viscosus, Prevotella intermedia, and Porphyromonas gingivalis. Therefore, any treatment for periodontitis and repairs should involve the inhibition of these microorganisms. Mirzaeei et al (2022) loaded tetracycline hydrochloride (TCH) into a polycaprolactone (PCL) solution for electrospinning into fibers. The resultant PCL/TCH fiber membrane showed antibacterial efficacy against all these species with 10 w/w% drug loading and greater inhibition zone with 20 w/w% loading. The highest efficacy was recorded against Actinomyces viscosus, and Porphyromonas gingivalis. With regards to the drug release profile, more than 60% of the drugs were released within the first 12 h and more than 90% was released after the next 144 h.
For a sustained release of metronidazole (MNA) in periodontitis treatment, Reise et al (2023) used coaxial electrospun poly(L-lactide-co-D,L-lactide) (PLA) fibers mats. Both the core and sheath material were PLA but MNA was only added to the core PLA solution. The resultant coaxial fibers (COAX) mat was compared with homogeneously distributed MNA in PLA nanofibers (HDN). The HDN showed an initial burst release but this was significantly reduced in the COAX which showed a more sustained release. Against F. nucleatum, both HDN and COAX fibers showed good inhibition from aliquots up to 168 h with COAX fiber showing greater inhibition than HDN after the first couple of hours. For P. gingivalis, antibacterial effect was shown up to 672?h for both HDN and COAX fibers however, COAX fibers showed significantly higher antibacterial effect at the time point. Cytocompatibility tests using human gingival fibroblasts (HGF) showed both mats to be compatible with COAX mat demonstrating significant higher numbers of viable cells. Therefore with a more sustained drug release from coaxial fibers, its antibacterial efficacy can be maintained with less stress on the cells.
Published date: 11 August 2015
Last updated: 09 January 2024
▼ Reference
-
Albuquerque M T P, Valera M C, Moreira C S, Breschiani E, Melo R M, Botiino M C. Effects of Ciprofloxacin-containing Scaffolds on Enterococcus faecalis Biofilms. Journal of Endodontics 2015; 41: 710.
-
Boyd S A, Su B, Sandy J R, Ireland A J. Cellulose Nanofibre Mesh for Use in Dental Materials. Coatings 2012; 2: 120.
Open Access
-
Deng X L, Xu M M, Li D, Sui G, Hu X Y, Yang X P. Electrospun PLLA/MWNTs/HA hybrid Nanofiber Scaffolds and Their Potential in Dental Tissue Engineering. Key Engineering Materials 2007; 330-332: 393.
-
Dodiuk-Kenig H, Lizenboim K, Roth S, Zalsman B, McHale W A, Jaffe M, Griswold K. Performance Enhancement of Dental Composites Using Electrospun Nanofibers. Journal of Nanomaterials 2008; 2008: 840254.
Open Access
-
Eap S, Becavin T, Keller L, Kokten T, Fioretti F, Weickert J L, Deveaux E, Benkirane-Jessel N, Kuchler-Bopp S. Nanofi bers Implant Functionalized by Neural Growth Factor as a Strategy to Innervate a Bioengineered Tooth. Adv. Healthcare Mater. 2014; 3: 386.
-
Fletcher J, Walsh D, Fowler C E, Mann S. Electrospun mats of PVP/ACP nanofibres for remineralization of enamel tooth surfaces. CrystEngComm 2011; 13: 3692.
-
Gao Y, Sagi S, Zhang L, Liao Y, Cowles D M, Sun Y, Fong H. Electrospun Nano-Scaled Glass Fiber Reinforcement of Bis-GMA/TEGDMA Dental Composites. J Appl Polym Sci 2008; 110: 2063.
-
Karatepe U Y, Ozdemir T. Improving mechanical and antibacterial properties of PMMA via polyblend electrospinning with silk fibroin and polyethyleneimine towards dental applications. Bioactive Materials 2020; 5: 510.
Open Access
-
Lee L W, Hsiao S H, Hung W C, Lin Y H, Chen P Y, Chiang C P. Clinical Outcomes for Teeth Treated with Electrospun Poly(ε-caprolactone) Fiber Meshes/Mineral Trioxide Aggregate Direct Pulp Capping. Journal of Endodontics 2015; 41: 628.
-
Liu J, Zou Q, Wang C, Lin M, Li Y, Zhang R, Li Y. Electrospinning and 3D printed hybrid bi-layer scaffold for guided bone regeneration. Materials & Design 2021; 210: 110047
Open Access
-
Mirzaeei S, Moghadam F, Asare-Addo K, Nokhodchi A. Design of a nanofibrous guided tissue regeneration carrier as a potential drug delivery system for tetracycline hydrochloride in the management of periodontitis. Journal of Drug Delivery Science and Technology 2022; 75: 103722.
Open Access
-
Nitt Pi, Palazzo B, Gallo N, Scalera F, Sannino A, Gervaso F. Smooth-rough asymmetric PLGA structure made of dip coating membrane and electrospun nanofibrous scaffolds meant to be used for guided tissue regeneration of periodontium. Polymer Engineering and Science 2022; 62: 2061
Open Access
-
Ravichandran R. Biomimetic Surface Modification of Dental Implant for enhanced Osseointegration. MEng Thesis. National University of Singapore 2009.
Open Access
-
Reise M, Kranz S, Guellmar A, Wyrwa R, Rosenbaum T, Weisser J, Jurke A, Schnabelrauch M, Heyder M, Watts D C, Sigusch B W. Coaxial electrospun nanofibers as drug delivery system for local treatment of periodontitis. Dental Materials 2023; 39: 132.
Open Access
-
Shah H V, Sandy J R, Ireland A J, Su B. Electrospinning of 2D and 3D silica nanofibres from a colloidal solution. Ceramics - Silikaty 2012; 56: 112.
Open Access
-
Tian M, Gao Y, Liu Y, Liao Y, Xu R, Hedin N E, Fong H. Bis-GMA/TEGDMA dental composites reinforced with electrospun nylon 6 nanocomposite nanofibers containing highly aligned fibrillar silicate single crystals. Polymer 2007; 48: 2720.
-
Yang M, Gao X, Shen Z, Shi X, Lin Z. Gelatin-assisted conglutination of aligned polycaprolactone nanofilms into a multilayered fibre-guiding scaffold for periodontal ligament regeneration. RSC Adv. 2019; 9: 507.
Open Access
-
Yang X, Yang F, Walboomers X F, Bian Z, Fan M, Jansen J A. The performance of dental pulp stem cells on nanofibrous PCL/gelatin/nHA scaffolds. J Biomed Mater Res 2010; 93A: 247.
▲ Close list
 ElectrospinTech
ElectrospinTech